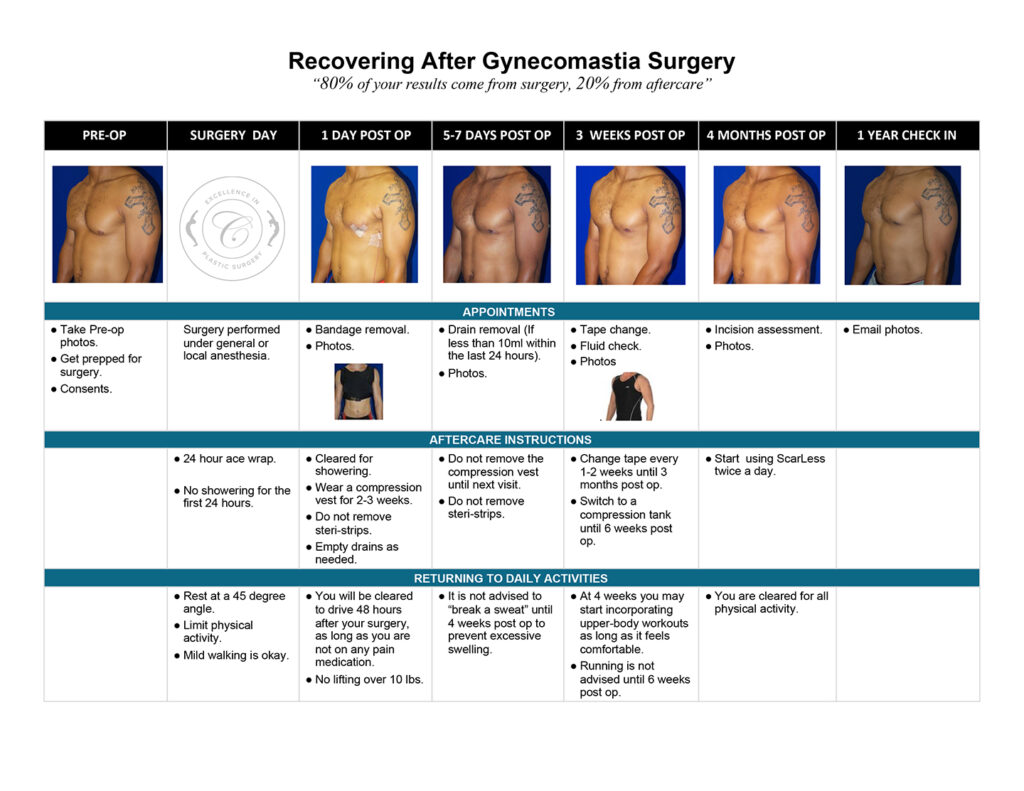
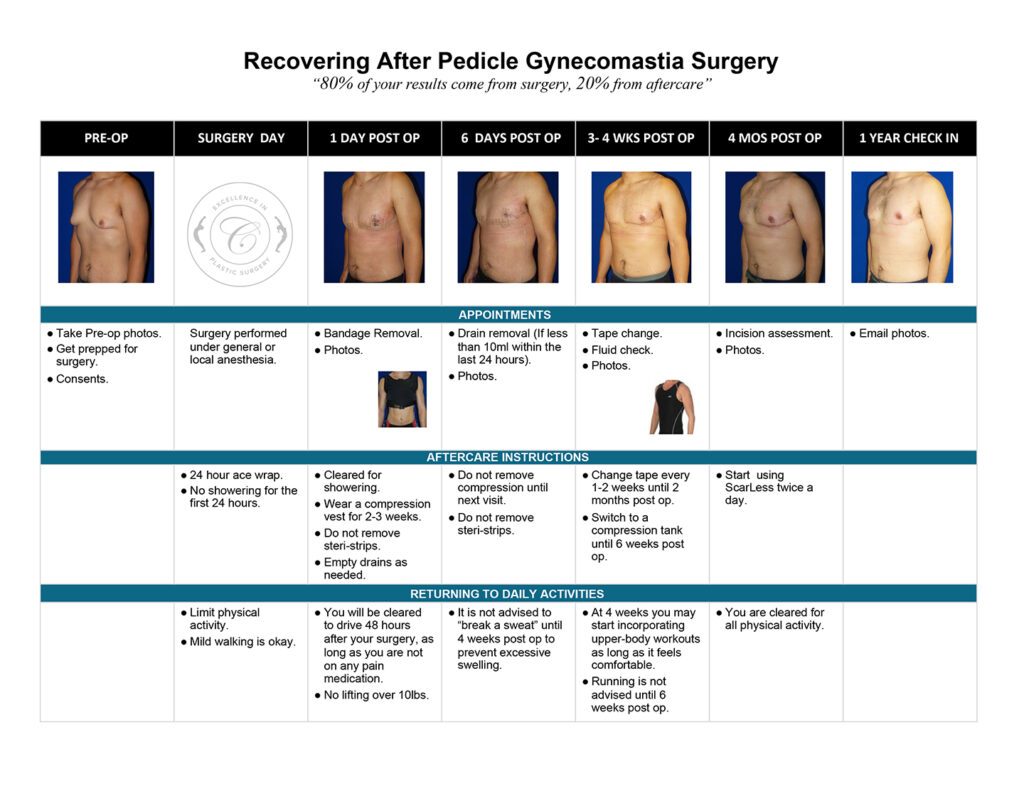
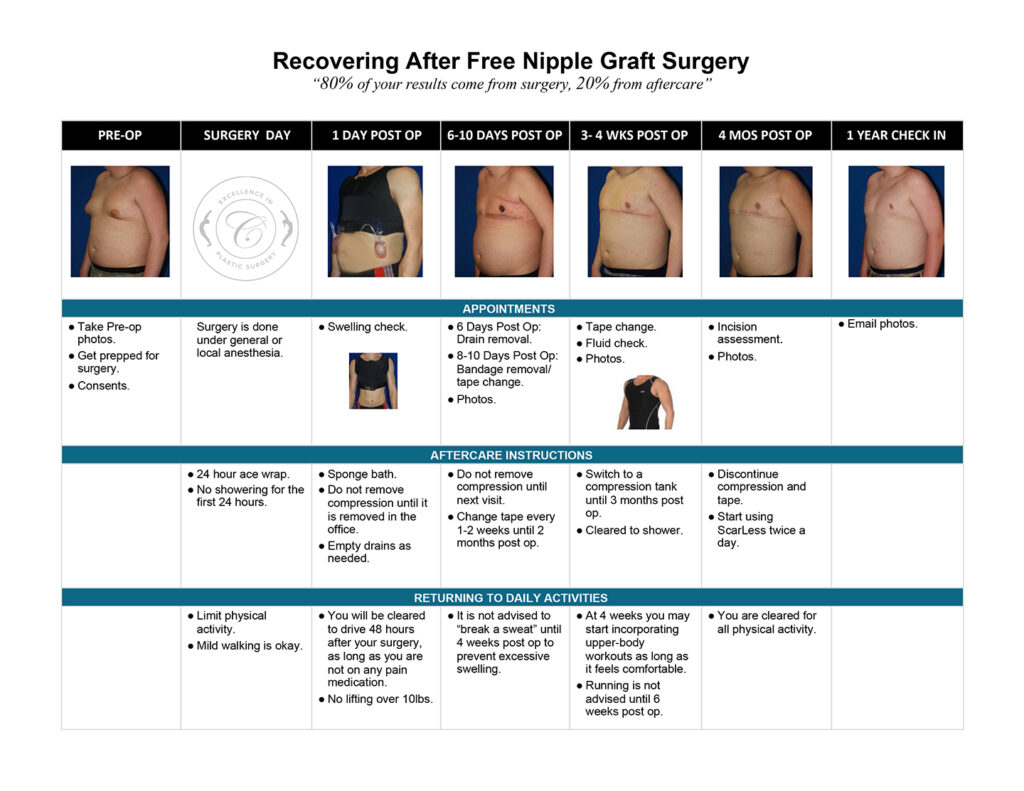
Gynecomastia Healing Process
The images below represent a standard gynecomastia healing process for each type of incision used (areola, extended periareolar, nipple repositioning/free nipple graft). The charts document the recovery timeline so you are familiar with what to expect at each stage after your gynecomastia surgery.
Possible Healing “Speed Bumps”
This section provides detailed information about some of the issues that can arise during the gynecomastia healing process following surgery. Some patients may experience none of the items listed, while others may experience one or more.
Use this information as a helpful resource should any of these apply to you. And, as always, please contact our office should you have a concern with your gynecomastia healing process.
- Asymmetric swelling
- Indentation after surgery
- Inverted nipples after surgery
- Rash/ Itching
- Stitch Abscess
- Wound breakdown
- Seroma
- Hematoma
- Constipation
- Muscle pain
- Scar progression
- Throat irritation after general anesthesia
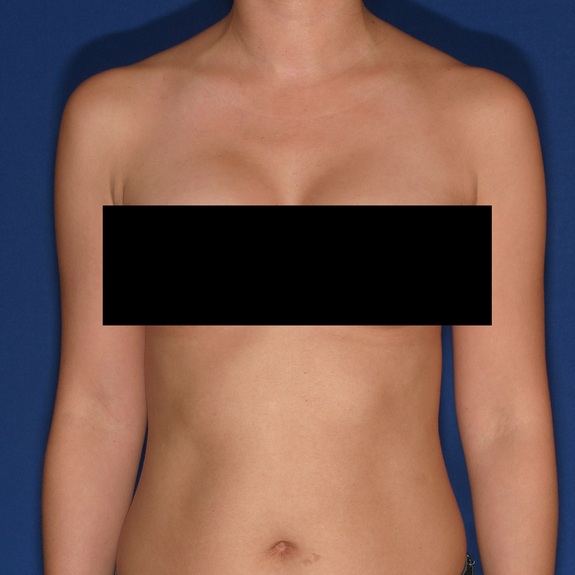
Asymmetric swelling
Symptoms:
- Nipples appear uneven
- Swelling more prominent on one side
- Bruising more prominent on one side
- Numbness on one side only
- Burning sensations on one side
- Muscle pain and limited arm motion on one side
- Indentation on one side only
- Inverted nipple on one side
Asymmetric healing progression







Causes:
Asymmetric swelling is the most common side effect you may encounter during the gynecomastia healing process. There are several factors that can cause this. Whenever dealing with pairs of any body part, you are likely to have asymmetric swelling. This can be caused by one muscle being stronger or more tense than the other, skin elasticity, more breast tissue on one side, fluid retention from the numbing medication, etc. This is all very normal and will get better as swelling goes down.
Treatment:
Compression is extremely important during the gynecomastia healing process and plays a big part in assisting the swelling and fluid to drain out as it promotes proper blood circulation, also helping to prevent blood clots from forming. Compression also insures the skin heals nice and flat to the chest wall. We also recommend icing for the first 2 weeks following surgery.
Indentation After Surgery
Symptoms:
Symptoms:
- Chest appears overcorrected
- Indent on one or both sides
- Chest indents when flexing muscles or elevating arms
- Chest can appear distorted
Indentation healing progression

Treatment:
There is no treatment needed since this will get better with time. In most patients this can take several months to fully flatten and smooth completely out.
Inverted nipples after surgery
Symptoms:
- Nipples inverted
- Nipples unable to get hard
Inverted nipples healing progression




Causes:
With almost any surgery involving incisions nerves get cut and can take several months to regain full sensation. Most patients will experience numbness during the gynecomastia healing process but may not notice other side effects depending on the area of operation.
With gynecomastia surgery, the incision is made around the areola to conceal the scar, and since nerves get cut, the patient will typically experience some degree of numbness after surgery often followed with inverted nipples due to the nerves being temporarily non-functioning. This can take weeks but more often months to fully regain sensation and the ability for the nipples to harden.
As nerves begin to re-attach you may also experience itching, burning sensations, tingling around the surgical area, or shooting pains. All of these sensations are normal in the healing process.
Treatment:
Always notify Dr. Cruise if you experience inverted nipples after surgery so we can document nerve sensation at each follow-up visit. There is no treatment since the nipples will correct on their own as the internal healing is complete.
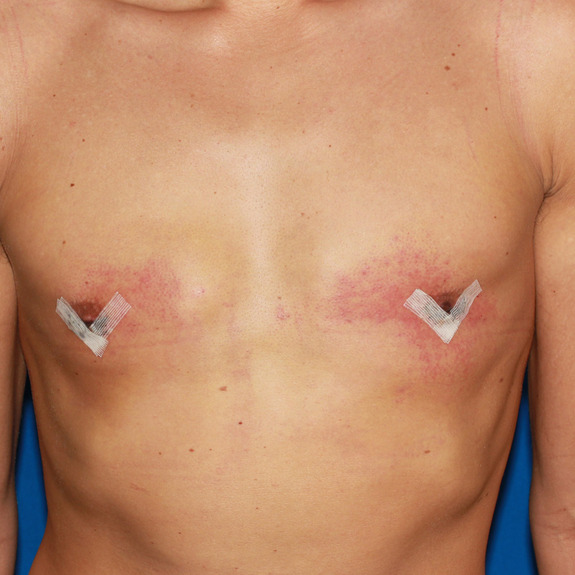
Rash/ Itching
Symptoms:
- Small pimple like bumps (often mistaken for body acne)
- Hives
- Redness followed with itching
- Excessive itching (minor itching can be normal with wound healing)
- Redness directly around surgical tape
- Blistering on the body or around surgical tape
Rash healing progression



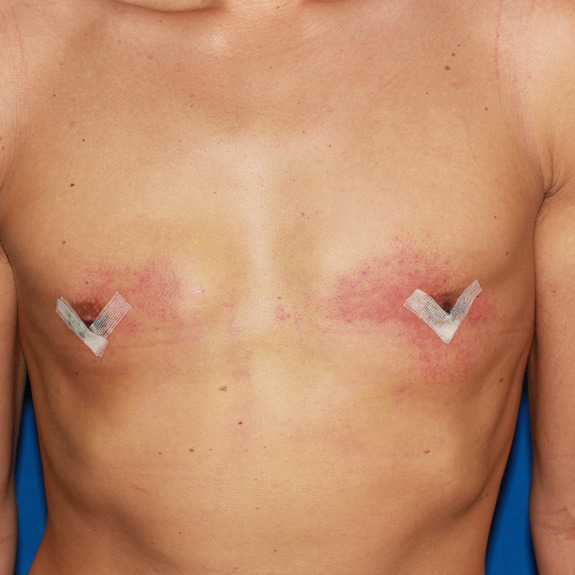

Causes:
Many patients may develop a rash after having surgery. This typically happens in the first few weeks following their procedure. A rash can be caused by an allergic reaction to medications, adhesive surgical tape, glue, topical creams, etc.
Treatment:
The first thing you will need to determine is if the rash is caused by an allergic reaction. For example, if you have redness and itching directly around your surgical tape it is most likely an allergic reaction and you will need to discontinue use.
If the rash is on a random area of the body or non-surgical site, it may be an allergy to a medication you are taking or one that you were taking. Allergic reactions often occur even after the offending agent is stopped.
The rash typically will get worse before it gets better. This is particularly concerning as people feel that it should go away immediately. The rash may persist for months and the hyper-pigmentation may last even longer. The good news is that it typically does go away completely.
All rashes should be reported to your doctor immediately. Treatment usually consists of applying a topical steroid and Benedryl.
Stitch abscess
Symptoms:
- Red swollen bump
- Oozing or discharge from the incision
- Opening on incision
- Whitehead on incision site
- Tenderness
- Hard string poking through incision site
Causes:
A stitch abscess is the body’s reaction to a foreign object. In this case, your body notices a stitch as a foreign body which can occur with both permanent and absorbable sutures. Because your body does not recognize this object it may want to get rid of it and push it towards the surface of the skin to dispose of it.
This is very common in recovery from excess breast tissue removal and does not affect your final results. Stitch abscesses can typically occur within the first 6 months after surgery.
Treatment:
If the stitch abscess is not dispensing any type of discharge or oozing on your surgical tape and it appears to be dry, it is okay to continue taping over it as normal. It will most likely flake off on its own within a few weeks.
If you do notice discharge coming from the stitch abscess, continue taping the entire incision except for that isolated area. You will need to apply a thin layer of Neosporin using a q-tip twice a day and put a band-aid over it. This may take anywhere from a few days to a few weeks to fully subside.
Once there is no more drainage on the bandaid, you may begin to apply surgical tape to the entire incision as before.
Wound Breakdown
Symptoms:
- Discharge or oozing from incision
- Visible opening on incision
- Tenderness
- Discoloartion around opening
- Burning sensation to skin around the area
- Fever
Wound Breakdown

after surgery.

scar was not affected in his final result.
Causes:
Causes:
A wound breakdown is an opening of the incision in an isolated area that the body is having a difficult time healing. Wound breakdowns usually occur within the first few weeks following surgery. It is important to notify your physician if you are experiencing a wound breakdown, so they can determine if the tissue looks healthy or if additional antibiotics may be needed to speed up the recovery.
Treatment:
If you have a wound breakdown, you will continue taping the entire incision except for this isolated area. You will need to apply Neosporin twice daily using a q-tip and place a large band-aid over it. This may take a few weeks to heal. Once the wound closes, you may notice the pigmentation slightly darker than the rest of the incision. This is normal and will fade out in time.
Seroma
Symptoms:
- Swelling in isolated area
- Water like effect when gently tapped with finger tips
- Soft to the touch
- Tenderness
- Asymmetric swelling
Seroma healing progression


Causes:
During surgery, saline solution is used to irrigate the area being operated on. Your body will naturally absorb this solution within the first few weeks following surgery. Sometimes a fluid pocket will form and will not allow the body to properly absorb it. This is known as a seroma.
Seromas are usually very easy to detect. With normal swelling, it will have a spongy feel when tapped with your fingertip. With a seroma, it will have a water wave effect when tapped with your finger.
Although a seroma is not an emergency, notify your doctor’s office promptly since you will need to have your physician aspirate it within 3-5 days of noticing the fluid collection. This does not affect your final results.
Treatment:
Ideally, seromas need to be aspirated by your physician within the first 3-5 days of noticing it. Depending on the patient, the fluid may return and may need to be drained 1-3 times before the seroma is completely healed.
Hematoma
Symptoms:
- Excessive swelling in a short period of time
- Skin will be very firm to the touch
- Pain
- Extreme amount of pressure
- Excessive bruising in a short period of time
Hematoma healing progression




Causes:
A hematoma is a localized collection of blood outside the blood vessels. When a blood vessel is damaged, blood can leak into the surrounding tissue. This blood may coagulate or clot. If you notice any of the symptoms above please contact your physician promptly.
Treatment:
Hematomas must be surgically removed by your physician. If you feel you may have a hematoma please contact your doctor immediately.
Constipation
Symptoms:
- Bloating
- Unable to make a bowel movement
- Abdominal discomfort
Causes:
Constipation is one of the most common things patients may encounter after surgery. We usually recommend taking stool softeners to help, but sometimes patients may require further treatment.
Constipation is caused by the anesthesia in your system after surgery. Most patients are able to have a bowel movement within the first few days after surgery. Those who are unable to make a bowel movement by day 3 should contact their physician for further treatment instructions.
Treatment:
If stool softeners have not worked, the next step would be to drink a glass of prune juice daily until on a normal cycle and take an over-the-counter suppository laxative. If still unable to make a bowel movement within 24 hours repeat instructions. If you are still unable to make a bowel movement by day 5 you need to go to an urgent care.
Muscle pain
Symptoms:
- Chest pain
- Difficulty with arm motion
Treatment:
There is no treatment needed as this is a normal part of the healing process. You may take tylenol for mild discomfort. If you have moderate to severe discomfort you may take your pain medication as directed by Dr. Cruise.
Scar progression
Symptoms:
- N/A
Scar progression








Causes:
With all scars, they will go through a recovery process. After the wound has closed together, the body will form scar tissue around the area which can turn the scar pink or purple in color. This phase may last a few months before starting to fade away to a skin tone.
You may also notice small bumps along the incision line after the wound closes. This is from both internal and external dissolvable sutures. These can take a few months to fully dissolve, as this happens you will notice the scar starting to flatten.
Treatment:
Scar formation can take up to 1-2 years before the process is fully completed. Dr. Cruise may recommend ScarLess if needed.
Throat irritation after general anesthesia
Symptoms:
- Sore throat
- Difficulty swollowing
- Visible white film in the back on tonsils and uvula
- Hard to talk after surgery
Causes:
The irritation will typically be at two different levels depending on the type of tube that was put in. For example, our anesthesiologist uses a Laryngeal Mask Airway (LMA) which is really nice because it is like a sponge that rests in the back of the throat. An LMA may cause irritation to the back of the throat (i.e uvula and tonsils).
The other type of tube is an Endotracheal Tube (ET tube). It goes all the way through the vocal cords and into the trachea. This tube can cause vocal cord irritation. This will make it hard to talk.
Treatment:
Always contact your physician to notify them if you are experiencing any of the above symptoms. Throat irritation is usually treated with frozen ice cream/ yogurt along with Chloraseptic Lozenges. Chloraseptic contains phenol which numbs the mouth and throat. It is OTC. Symptoms usually start getting better in as little as 3-10 days after starting treatment.








