Los Angeles Gynecomastia
Welcome to LA Gynecomastia
Los Angeles Gynecomastia (a.k.a. LAGynecomastia.com) was developed to provide all of the information needed when researching about gynecomastia and the available surgical options. Over the past decade, Dr. Cruise’s practice has been largely devoted to the treatment of gynecomastia, and he has become known as one of the top gynecomastia surgeons in the country. Dr. Cruise is regarded as an authority within this unique subspecialty. LA gynecomastia reflects his dedication to the treatment of gynecomastia.
Gynecomastia Overview
The first thing men want to know is “What is Gynecomastia?” followed by “What causes it?”
Gynecomastia is defined as excess excess development of male breast tissue that enlarges or swells due to reduced testosterone or increased estrogen. The breast tissue is usually benign. Gynecomastia can affect one or both male breasts. Gynecomastia is only a problem if it negatively affects your life, in which case surgical treatment is available to permanently get rid of it.
Causes typically include puberty, hormonal changes, aging, taking certain medications or drugs, certain health conditions, and genetic predisposition. Some men will never know the exact cause of their enlarged male breasts.
Approximately 50-70% of normal pubescent teenage boys experience some degree of change in their breasts. In most cases it will resolve on its own by adulthood.
Cruise Classification System
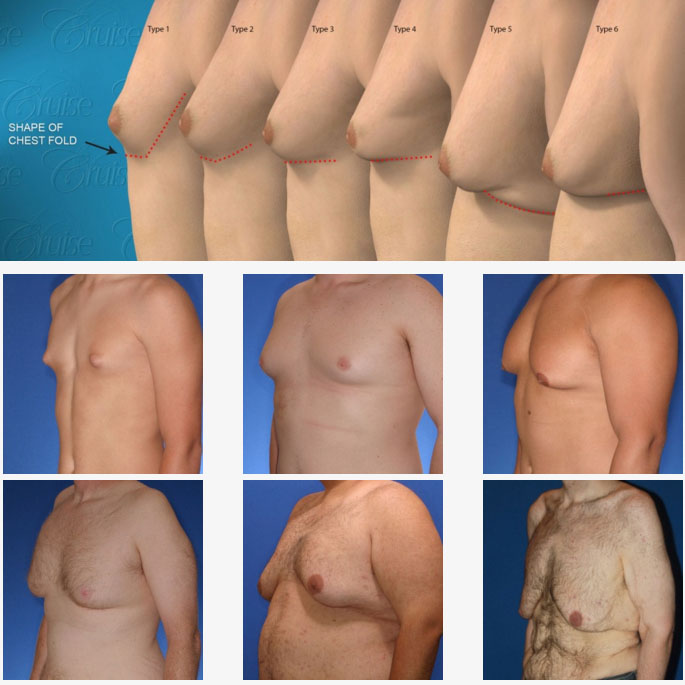
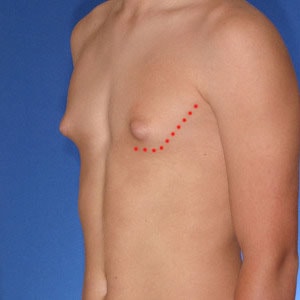
Dr. Cruise created the “Cruise Classification System” to demonstrate how each type of gynecomastia differs and to show what treatment option is best suited to achieve optimal results.
Cruise Classification System – 6 Types of Gynecomastia
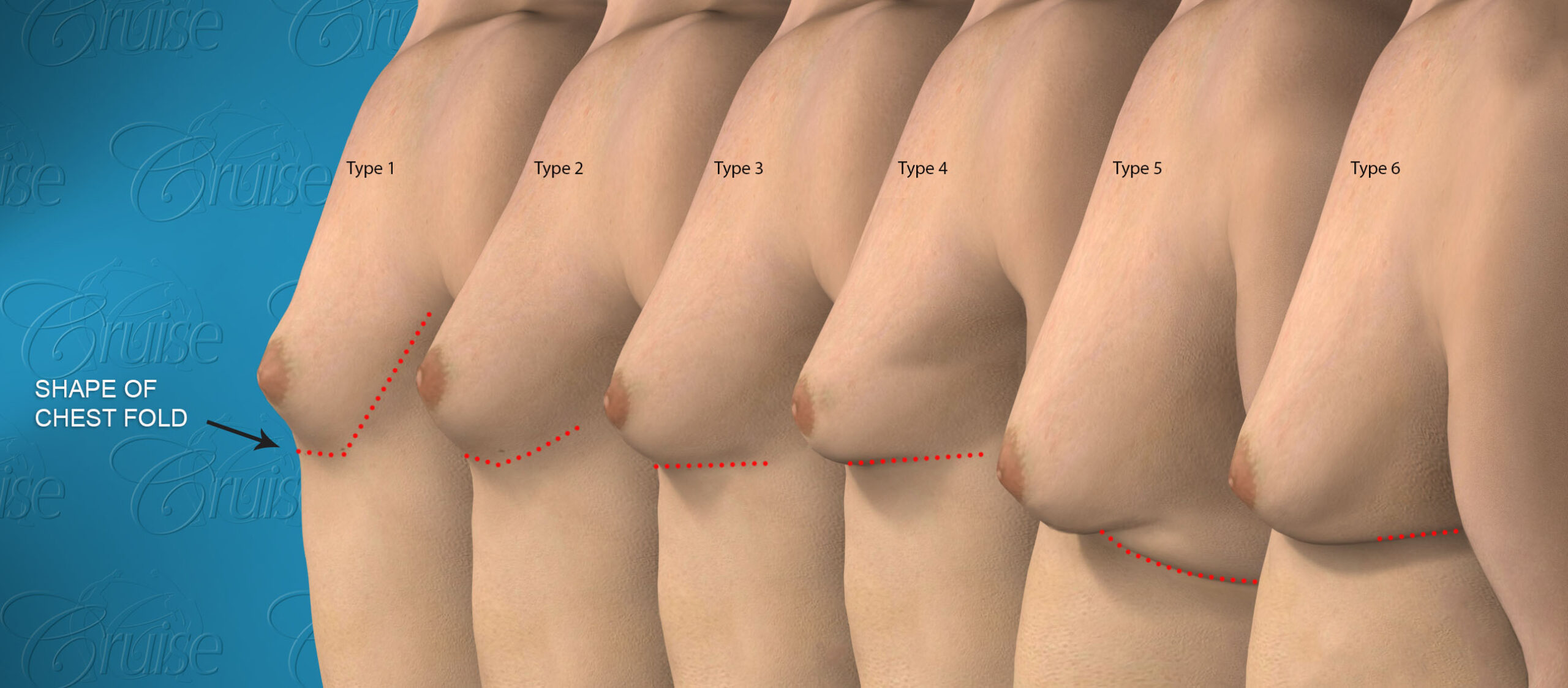
Notice the progressive increase in skin laxity. This excess skin will change the type of surgery necessary to properly correct the problem.

- Type 1


- Type 2


- Type 3

- Type 4


- Type 5


- Type 6
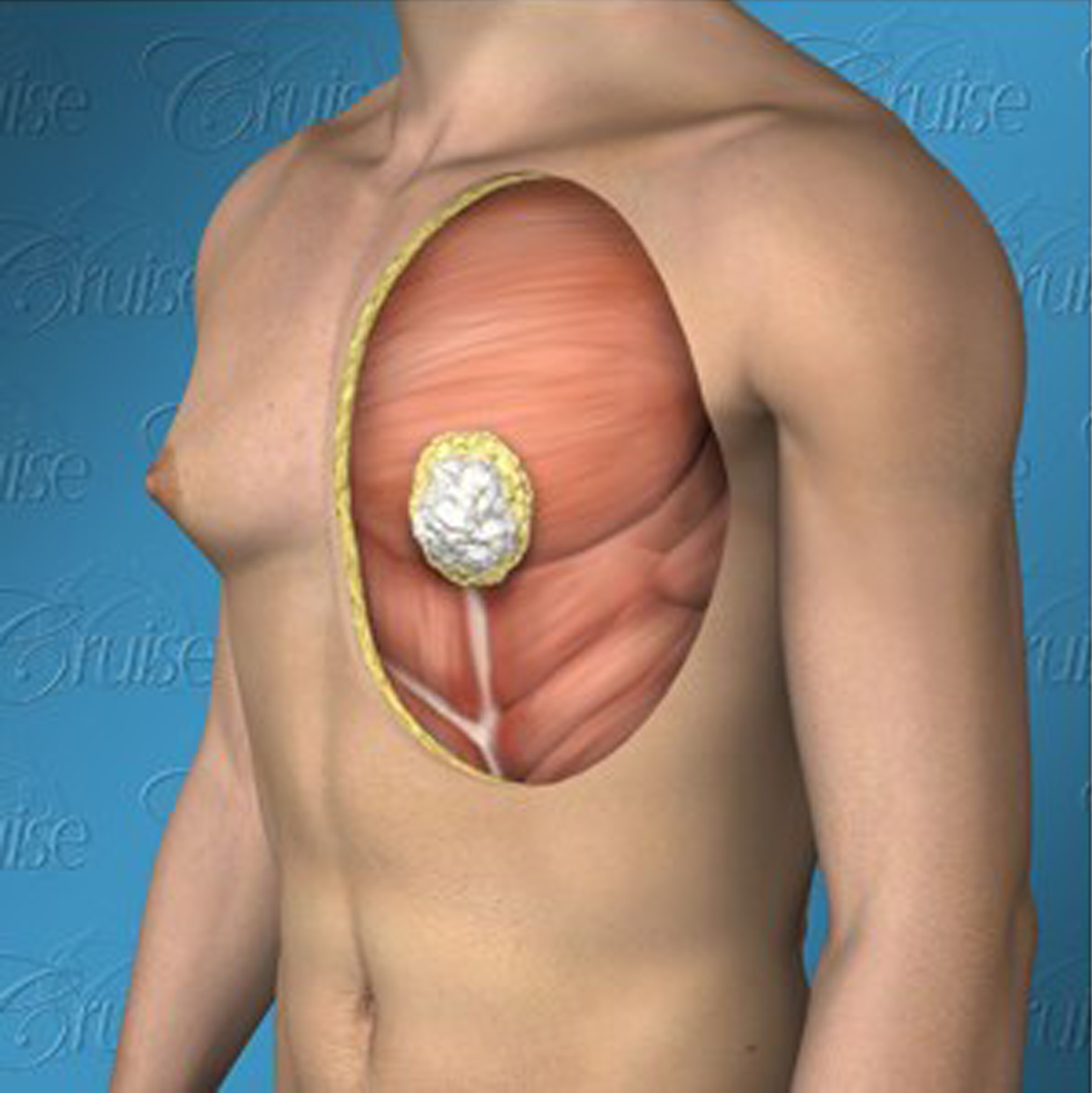
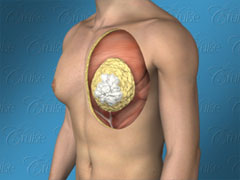
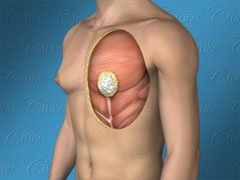
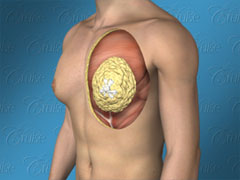
Components of Gynecomastia
There are typically three primary underlying reasons for the breast enlargement. There can be one issue present or a combination.
- Excess breast tissue
- Excess fat
- Excess skin
Dr. Cruise categorizes the breast enlargement into 5 components based on what is actually causing it.
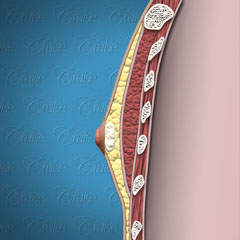
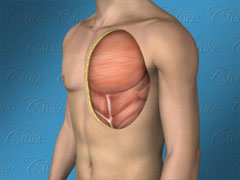
When looking at the graphic below, note that:
White = glandular, breast tissue
Yellow = fatty tissue
Saggy and breast roll = demonstrate skin laxity
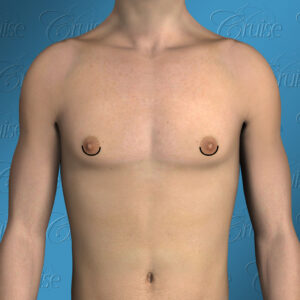
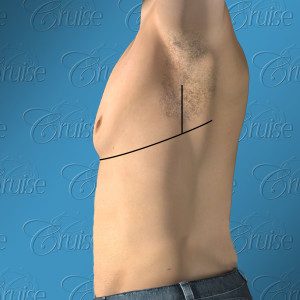
The Ideal Male Chest

Dr. Cruise breaks down the 8 areas of the upper body which need to be evaluated to determine how to achieve the optimal result for each patient.
- Chest shape – masculine, flat, defined
- Nipple position
- Areola size – projection, shape
- Pec. border definition
- Arm pit
- Fat pockets – pre-axillary, axillary, breast roll
- Breast roll
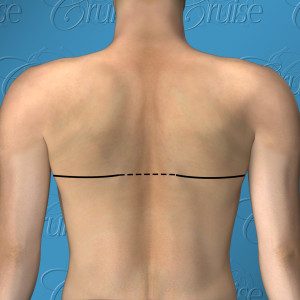
- Back roll
Gynecomastia Surgical Treatment
The inferior crescent incision is the most commonly used by Dr. Cruise with Type 1 & Type 2 gynecomastia. The superior crescent incision is used when the nipple is near the pec. border and a small amount of elevation is needed to ensure the nipple doesn’t migrate downward when breast tissue is removed.
In most cases, Dr. Cruise uses both the inferior and superior crescent incisions for Type 3 gynecomastia. He uses this technique instead of the traditional donut lift, which can cause puckering around the areola.
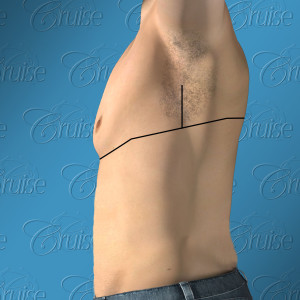
Types 4 – 5

Chest tightening w/ nipple repositioning or free nipple graft
Extended chest lift w/ axillary pleat
Type 4 gynecomastia Dr. Cruise uses either chest tightening w/ nipple repositioning or a free nipple graft. Nipple repositioning maintains blood and nerve supply during surgery, while FNG completely removes the nipple. FNG is used when there is significant tissue that needs to be removed.
Type 5 gynecomastia often includes an extended chest lift/axillary pleat, which is well hidden within the armpit area. The benefits include more dramatic skin tightening and fat removal, which creates more definition not only from the front view, but the side view as well.
Type 6 gynecomastia uses the same incision shown above for Type 4 & 5 from the front view. A chest lift is performed with either nipple repositioning or free nipple graft, along with an incision which continues around the side to the back. The incision will go as far as the back roll goes. If necessary, a circumferential incision will be used as represented by the dotted lines.
Gynecomastia Before & After Photos
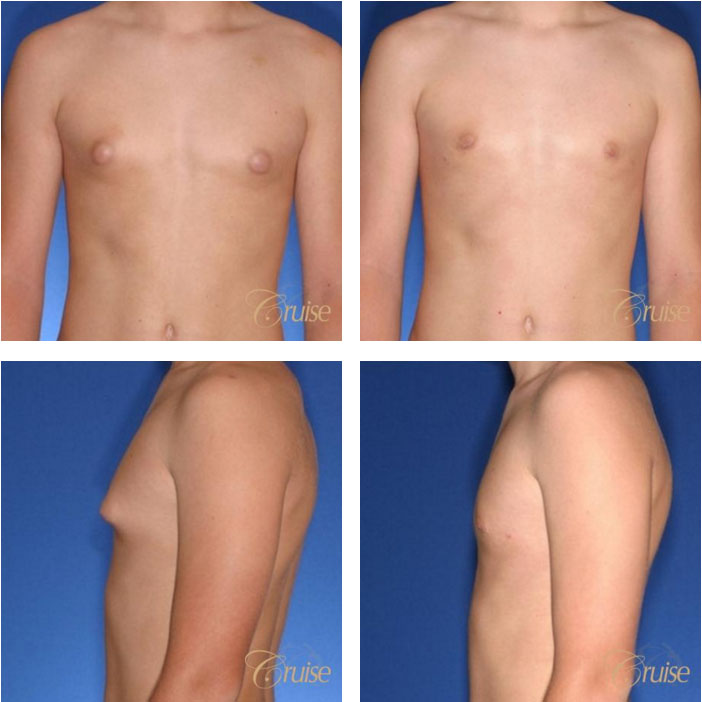
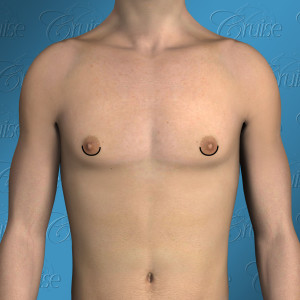
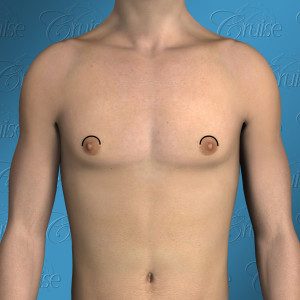
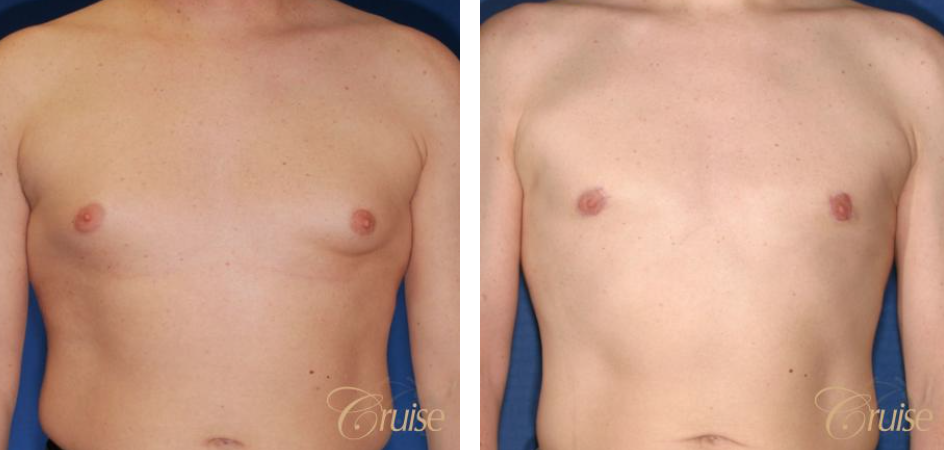
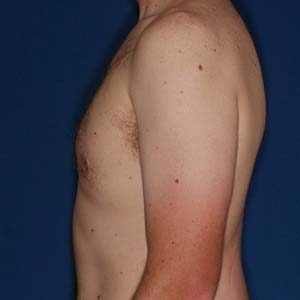
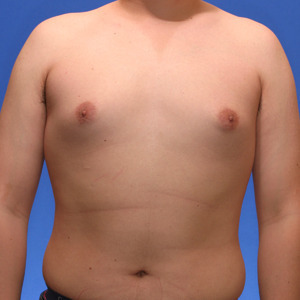
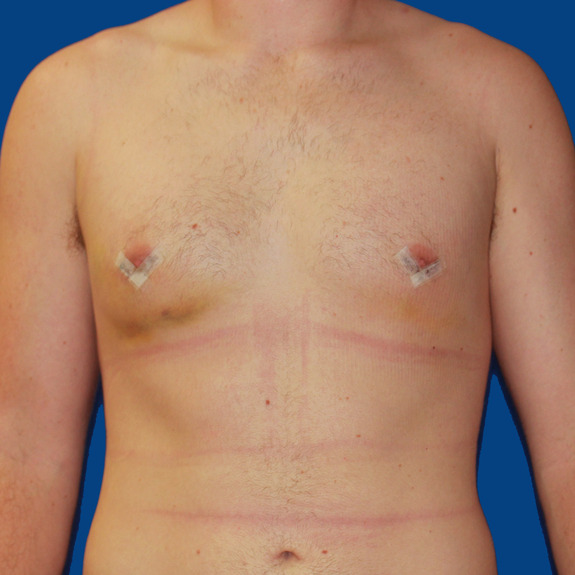
Los Angeles Gynecomastia Example 1
Surgery on a 14 year old teenager. Patient had liposuction and breast tissue excision to correct his gynecomastia.

Before

After

Before

After
Los Angeles Gynecomastia Example 2
Patient had liposuction and breast tissue excision to correct his gynecomastia.

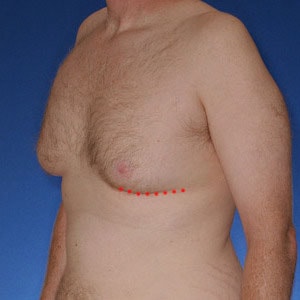
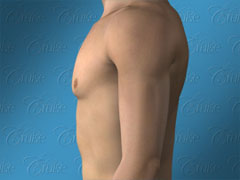
Before

After

Before

After
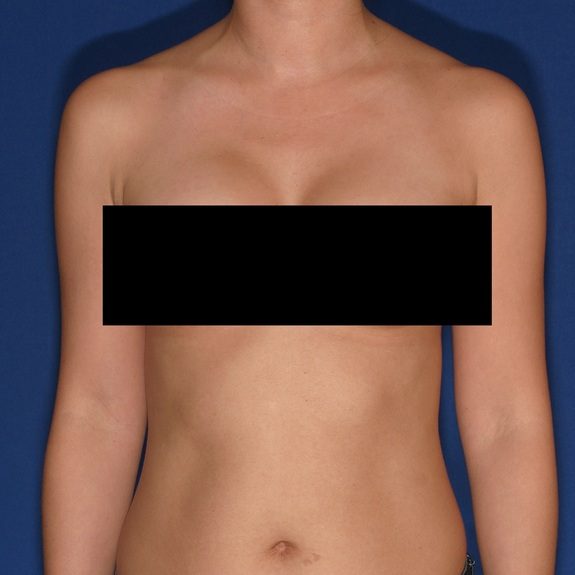
Los Angeles Male Breast Reduction Example 3
27 year old patient had liposuction and breast tissue excision to correct his gynecomastia.

Before

After

Before

After
Los Angeles Gynecomastia Example 4
Gynecomastia correction on a 33 year old. Patient had liposuction, breast tissue excision, as well as some skin removed via Donut Lift to correct his gynecomastia.

Before

After

Before
After
Los Angeles Gynecomastia Example 5
20 year old patient had liposuction and breast tissue excision to correct his gynecomastia.

Before

After

Before

After
Los Angeles Puffy Nipple Example 6
This 18 year-old patient had liposuction and breast tissue excision to correct his puffy nipples.
Before

After

Before

After
For more gynecomastia before and after photos, visit our comprehensive photo gallery.
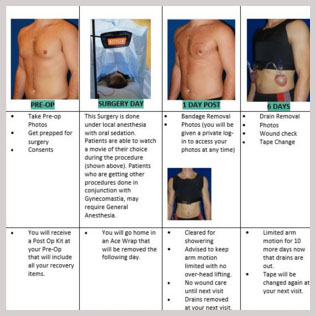
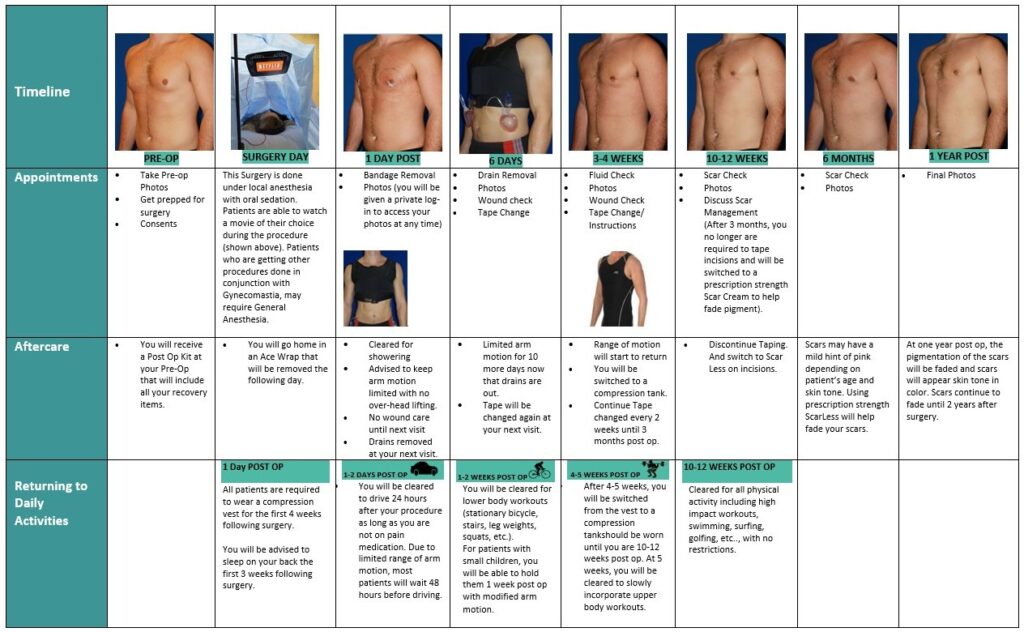
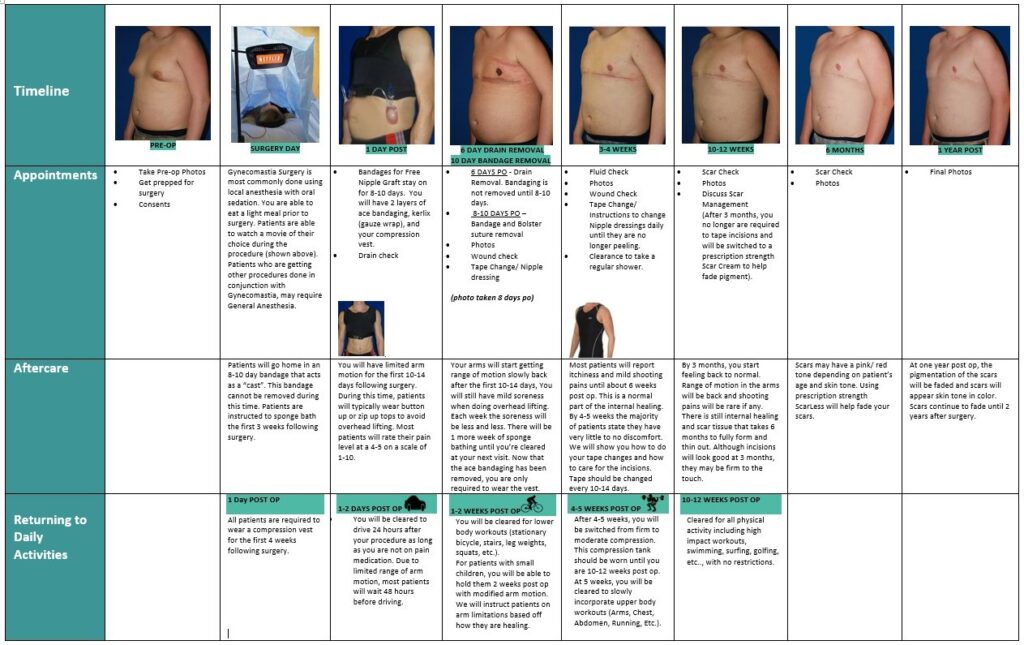
Recovery Timeline
Areola Incisions (Types 1-3)
Chest lift (Types 4-6)
Specific healing concerns
- Asymmetric swelling
- Indentation after surgery
- Inverted nipples after surgery
- Rash/ Itching
- Stitch Abscess
- Wound breakdown
- Seroma
- Hematoma
- Constipation
- Muscle pain
- Scar progression
Asymmetric swelling
Symptoms:
- Nipples appear uneven
- Swelling more prominent on one side
- Bruising more prominent on one side
- Numbness on one side only
- Burning sensations on one side
- Muscle pain and limited arm motion on one side
- Identation on one side only
- Inverted nipple on one side
Asymmetric healing progression







Causes: Asymmetric swelling is the most common side affect you may encounter after surgery. There are several factors that can cause this. When ever dealing with two’s of any body part you are likely to have asymmetric swelling. This can be caused by one muscle being stronger or more tense than the other, skin elasticity, more breast tissue on one side, fluid retention from the numbing medication, etc. This is all very normal and will get better as swelling goes down.
Treatment: Compression is extremely important after surgery and does a big part in assisting the swelling and fluid to drain out. Compression also insures the skin heals nice and flat to the chest wall. We also recommend icing for the first 2 weeks following surgery.
Indentation after surgery
Symptoms:
- Chest appears overcorrected
- Indent on on or both sides
- Chest indents when flexing muscles or elevating arms
- Chest can appear distorted
Indentation healing progression
This patient has an indentation on the left breast to the left of the areola.

the indentation has flattened out and chest appears smooth and flat.
Treatment: There is no treatment needed since this will get better with time. In most patients this can take several months to fully flatten and smooth completely out.
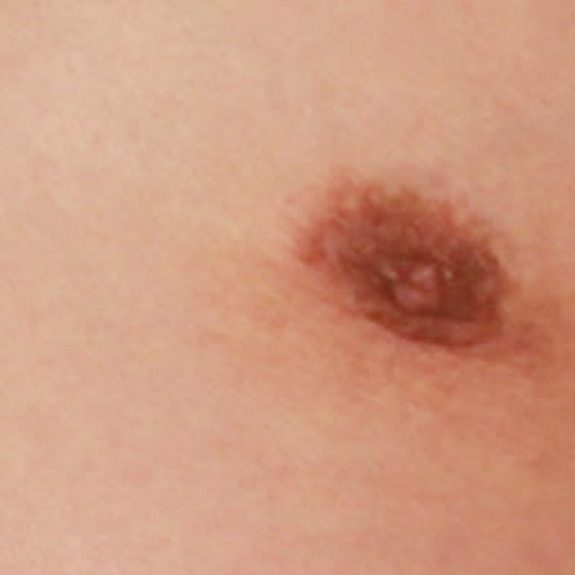
Inverted nipples after surgery
Symptoms:
- Nipples inverted
- Nipples unable to get hard
Inverted nipples healing progression

patient experienced inverted nipples post surgery.

after his last visit, the nipples regained nerve sensation and inverted nipples corrected on their own.

patient had an inverted nipple on the left side only during his healing process.

after the internal swelling had decreased and nerve sensation returned, the left nipple was corrected on its own during the healing process.
Causes: With almost any surgery involving incisions nerves get cut and can take several months to regain full sensation. Most patients will experience numbness following surgery but may not notice other side effects depending on the area of operation. With gynecomastia surgery the incision is made around the areola to conceal the scar, since nerves get cut the patient will typically experience some degree of numbness after surgery and often followed with inverted nipples due to the nerves being temporary non-functioning. This can take weeks but more often months to fully regain sensation and the ability for the nipples to harden. As nerves begin to re-attach you may also experience itching, burning sensations, tingling around surgical area, or shooting pains. All of these sensations are normal in the healing process.
Treatment: Always notify Dr. Cruise if you experience inverted nipples after surgery so we can document nerve sensation at each follow up visit. There is no treatment since the nipples will correct on their own as the internal healing is complete.
Rash/Itching
Symptoms:
- Small pimple like bumps (often mistaken for body acne)
- Hives
- Redness followed with itching
- Excessive itching (minor itching can be normal with wound healing)
- Redness directly around surgical tape
- Blistering on the body or around surgical tape
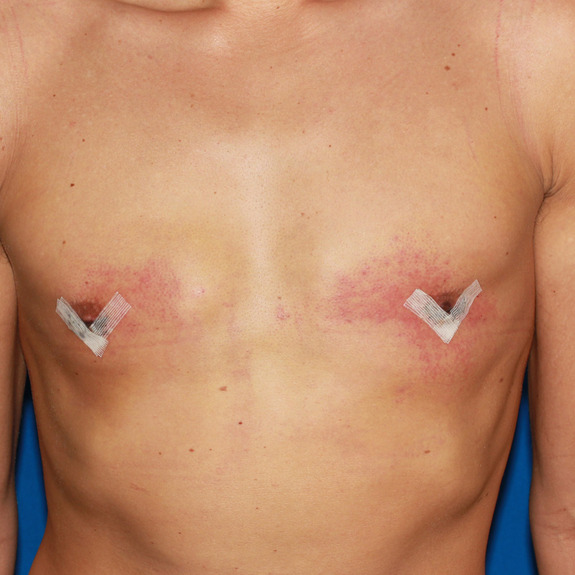
Rash healing progression

Example of an allergic reaction to the surgical tape. Notice the irritation is isolated to the area where the tape was in place.
the rash is now gone and incision is still healing right on track. The rash did not have an affect on the final result.

This rash occured and was most likely a reaction to medication or cream. Notice the rash is outside the surgical area.

patient developed a rash around his surgical tape.

patient was advised to discontinue surgical tape. and rash is no longer present.
Causes: Many patients may develope a rash after having surgery. This typically happens in the first few weeks following their procedure. A rash can be caused by an allergic reaction to medications, adhesive surgical tape, glue, topical creams, etc.
Treatment: The first thing you will need to determine is if the rash is caused by an allergic reaction. For example, if you have redness and itching directly around your surgical tape it is most likely an allergic reaction and you will need to discontinue use. If the rash is on a random area of the body or non surgical site, it may be an allergy to a medication you are taking or one that you were taking. Allergic reactions often occur even after the offending agent is stopped. The rash typically will get worse before it gets better. This is particularly concerning as people feel that it should go away immediately. The rash may persist for months and the hyperpigmentation may last even longer. The good news is that it typically does go away completely.
All rashes should be reported to your doctor immediately. Treatment usually consists of applying a topical steroid.
Stitch abscess
Symptoms:
- Red swollen bump
- Oozing or discharge from the incision
- Opening on incision
- Whitehead on incision site
- Tenderness
- Hard string poking through incision site
Causes: A stitch abscess is the body’s reaction to a foreign object (a foreign body is any object originating outside the body). In this case, your body notices a stitch as a foreign body which can occur with both permanent and absorbable sutures. Because your body does not recognize this object it may want to get rid of it and push it towards the surface of the skin to dispose of it. This is very common in recovery and does not affect your final results. Stitch abscesses can typically occur within the first 6 months after surgery.
Treatment: If the stitch abscess is not dispensing any type of discharge or oozing on your surgical tape and it appears to be dry, it is okay to continue taping over it as normal. It will most likely flake off on its own within a few weeks. If you do notice discharge, coming from the stitch abscess, continue taping entire incision except for that isolated area. You will need to apply a thin layer of neosporin using a q-tip twice a day and put a band aid over it. This may take anywhere from a few days to a few weeks to fully subside. Once there is no more drainage, on the bandaid, you may begin to apply surgical tape to the entire incision as before.
Wound breakdown
Symptoms:
- Discharge or oozing from incision
- Visible opening on incision
- Tenderness
- Discoloartion around opening
- Burning sensation to skin around the area
- Fever
Wound Breakdown


Causes: A wound breakdown is an opening of the incision in an isolated area that the body is having a difficult time healing. Wound breakdowns usually occur within the first few weeks following surgery. It is important to notify your physician if you are experiencing a wound breakdown, so they can determine if the tissue looks healthy or if additional antibiotics may be needed to speed up the recovery.
Treatment: If you have a wound breakdown, you will continue taping the entire incision except this isolated area. You will need to apply a cream twice daily using a q-tip and place a large band aid over it. This may take a few weeks to heal. Once the wound closes, you may notice the pigmentation slight darker than the rest of the incision. This is normal and will fade out in time. See photo below for example before and after wound breakdown.
Seroma
Symptoms:
- Swelling in isolated area
- Water like effect when gently tapped with finger tips
- Soft to the touch
- Tenderness
- Asymmetric swelling
Seroma healing progression


Causes: During surgery saline solution is used to irrigate the area being operated on. Your body will naturally absorb this solution within the first few weeks following surgery. Sometimes a fluid pocket will form and will not allow the body to properly absorb it. This is known as a seroma. Seromas are usually very easy to detect. With normal swelling it will have a spongy feel when tapped with your fingertip. With a seroma, it will have a water wave effect when tapped with you finger. Although a seroma is not an emergency, notify your doctors office promptly since you will need to have your physician aspirate it within3-5 days of noticing the fluid collection. This does not affect your final results.
Treatment: Ideally seromas need to be aspirated by your physician within the first 3-5 days of noticng it. Depending on the patient, the fluid may return and may need to be drained 1-3 times before seroma is completely healed.
Hematoma
Symptoms:
- Excessive swelling in a short period of time
- Skin will be very firm to the touch
- Pain
- Extreme amount of pressure
- Excessive bruising in a short period of time
Hematoma healing progression




Causes: A hematoma is a localized collection of blood outside the blood vessels. When a blood vessel is damaged blood can leak into the surrounding tissue. This blood may coagulate or clot. If you notice any of the symptoms below please contact your physician promptly.
Treatment: Hematomas must be surgically removed by your physician. If you feel you may have a hematoma please contact your doctor immediately.
Constipation
Symptoms:
- Bloating
- Unable to make a bowel movement
- Abdominal discomfort
Causes: Constipation is one of the most common things patients may encounter after surgery. We usually recommend taking stool softeners to help, but sometimes patients may require further treatment. Constipation is caused by the anesthesia in your system after surgery. Most patients are able to have a bowel movement within the first few days after surgery. Those who are unable to make a bowel movement by day 3 should contact their physician for further treatment instructions.
Treatment: If stool softeners have not worked, the next step would be to drink a glass of prune juice daily until on a normal cycle and take an over the counter suppository laxative. If still unable to make a bowel movement within 24 hours repeat instructions. If you are still unable to make a bowel movement by day 5 you need to go to an urgent care.
Muscle pain
Symptoms:
- Chest pain
- Difficulty with arm motion
Treatment: There is no treatment needed as this is a normal part of the healing process. You may take tylenol for mild discomfort. If you have moderate to severe discomfort you may take your pain medication as directed by Dr. Cruise.
Scar progression
Scar progression timeline
Examples of what scar progression looks like during the healing process.

2 weeks post op

7 weeks post op

3 weeks post op

6 months post op

2 weeks post op

2 months post op


Causes: With all scars, they will go through a formation process. After the wound has closed together the body will form scar tissue around the area which can turn the scar pink or purple in color. This phase may last a few months before starting to fade away to a skin tone. You may also notice small bumps along the incision line after the wound closes. This is from both internal and external dissolvable sutures. These can take a few months to fully dissolve, as this happens you will notice the scar starting to flatten.
Treatment: Scar formation can take up to 1-2 years before its completed. If needed, Dr. Cruise may recommend ScarLess® scar gel, which is available at our office.
For Significant Others/Parents
The stigma associated with gynecomastia keeps many men from sharing the pain they may be experiencing as a result of their female appearing breasts. It isn’t always obvious what your loved one may be feeling. Those who are most deeply affected go to great lengths to suffer alone.
As a significant other or parent, it is important to pay close attention to any signs which may point to your loved one struggling with serious issues resulting of his gynecomastia.
Some of the signs to watch for:
- Avoids social settings
- Not wanting to take his shirt off around other people
- Wearing baggy clothing, wearing extra bulky clothing in warmer climates
- Depressed, negative, or hopeless
- Avoids physical contact
- Obsessed with working out and/or dieting
- Gaining weight, not working out and eating poorly
If you determine there is a problem, don’t force your loved one to open up to your right away. You may want to start by saying something like “I noticed you seem less motivated lately. Is everything ok?” or “You used to enjoy going to beach, but seem to avoid it lately. Is there something going on you would like to talk about?”